





"The good news is that when compared to other developing countries, where the use of antibiotics is rife and communities can buy these medicines without prescriptions, South Africa is doing well in terms of policies and a strategy to combat future resistance to antibiotics," says Dr Kim Faure, South Africa's co-ordinator for CDDEP. "South Africa's data shows that the resistance of organisms in our hospitals and communities is not as high as some other countries in the world but usage of antibiotics is on the rise with potential for multi drug-resistant strains of bacteria to grow."
The report demonstrates that the greatest increase in antibiotics use was in the BRICS countries, with South Africa's consumption increasing over 60% in the space of 10 years, signalling increased prescribing in both the hospital and community settings. "The more we use antibiotics, the more resistance will increase. Misuse or over-prescribing of antibiotics is also a problem because resistance that develops in one person can spread to others and therefore affects everyone."
This is the first time The State of The World's Antibiotics report included data from South Africa - both the public and private sectors - and other developing countries. "South Africa has an excellent national strategy in place and is one of the few developing countries that has started a national surveillance system to monitor resistance trends and inform policy development and clinical decision-making."
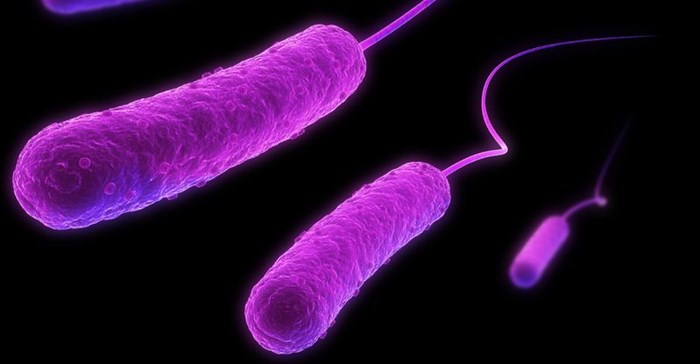
However, the report did note that despite these measures, resistance to the three key infectious organisms measured in the report remains high. "In more than a quarter of cases, we're seeing resistance to some of the most dangerous infectious organisms to last-resort antibiotics," says Faure. These include 27% of cases of Escherichia coli (often referred to as E-coli) organisms, a common cause of urinary tract infections and 30% of Staphylococcus aureus cases, a 'super bug' that causes skin and soft tissue infections. There was also a worrying increase between 2012 and 2014 from 3.8% to 4.2% of cases of resistance to Klebsiella pneumoniae (KP), to antibiotics considered last resort, which can cause life-threatening infections in patients in hospitals.
These findings were released via the CDDEP's ResistanceMap, an interactive online tool that allows users to track the latest global trends in drug resistance in 39 countries and antibiotic use in 69 countries.
Faure says changing patient and doctors' mind-sets is crucial. "It's about educating the public not to pressurise doctors into prescribing antibiotics for minor ailments and viral infections such as flu, as well as using antibiotics only when prescribed and for the duration and frequency they are prescribed."
Gross antibiotic overuse can accelerate antibiotic resistance, with the growing possibility that the few antibiotics we have left will no longer be effective and patients will die from simple infections that cannot be treated. The CDDEP says antibiotic use can be rationalised by reducing the need for antibiotics through better public health, including better sanitation and the use of vaccines to control infectious diseases. Curbing unnecessary use of antibiotics - especially in the community setting - as well as improving access where use is warranted, is also essential. Since many farmers use antibiotics to optimise meat production, monitoring usage in the agricultural sector should be a priority.
Importantly, for at least some antibiotics, resistance levels decrease with declining use, conserving and even recovering some antibiotic effectiveness. According to The State of The World's Antibiotics, 2015, in some countries where antibiotic stewardship has taken hold and public health is good, antibiotic resistance levels have stabilised or declined: and when antibiotic use declines, the prevalence of antibiotic-resistant bacteria tends to fall.
While there has been much emphasis on offering incentives for new antibiotic development to pharmaceutical companies, the report suggests there needs to be more focus on policies that encourage antibiotic conservation. "The transformation will not be easy, but social norms can and do change-witness the change in attitudes toward cigarette smoking. Each of us doing our part to conserve antibiotics and use them appropriately can start the process," the report says. Faure says South Africa is looking at conserving antibiotics in hospital and community settings as well as in the agricultural sector and aims to target both healthcare providers and the public.
"It's not too late to encourage people to change how they view and use antibiotics. It is possible not only to conserve the current effectiveness of existing antibiotics, but even to reclaim some of the effectiveness that has been lost. This is essential given that the pipeline of new drugs is limited," concludes Faure.